
You don't have to live with it
We can help you
Conquer low back pain
Next to the common cold, low back pain is the most frequent complaint among those who seek medical advice. Low back pain is a very common and complex disease of the spine, and it is one of the leading causes of chronic pain.
Pain in the lower back is a common concern, affecting up to 90% of people at some point in their lifetime. Up to 50% will have more than one episode. Low back pain is not a specific disease, rather it is a symptom that may occur from a variety of processes.
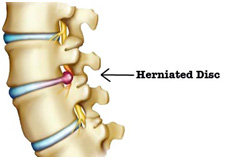 Prolapsed Intervertebral Disc is the major cause of LBP/sciatica not responding to conservative line of Treatment
Prolapsed Intervertebral Disc is the major cause of LBP/sciatica not responding to conservative line of Treatment
Radicular pain/ axial lowback pain
Radicular pain : lumbar disc herniation, nerve root compression
Axial lowback pain
COMMON CAUSES OF LOW BACK PAIN
DISCOGENIC PAIN
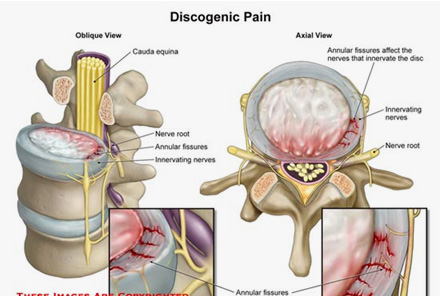 Discogenic pain is defined as pain originating from the intervertebral disc. It is nonradicular and may occur in the absence of spinal deformity, instability and signs of neuronal tension. Although the external outline of the disc may remain intact there are many pathologic processes including annular tears, degeneration, endplate injury, and inflammation, that can cause sensitization and stimulate nociceptors within the disc itself independent of nerve root involvement.
Discogenic pain is defined as pain originating from the intervertebral disc. It is nonradicular and may occur in the absence of spinal deformity, instability and signs of neuronal tension. Although the external outline of the disc may remain intact there are many pathologic processes including annular tears, degeneration, endplate injury, and inflammation, that can cause sensitization and stimulate nociceptors within the disc itself independent of nerve root involvement.
Pain is increased with sitting, flexion, coughing, sneezing or activities that increase intradiscal pressure such as straining and improvement with recumbency.
The most common presentation is axial back pain associated with decreased range of motion of the spine, especially with flexion. Palpation usually reveals midline tenderness near the affected segments.
LUMBAR FACET PAIN
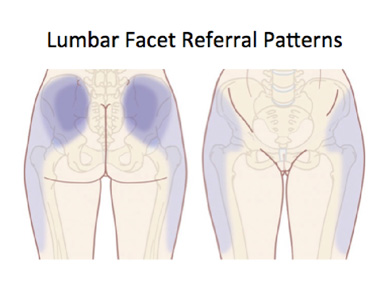 Lumbar facet joint-mediated pain tends to present as a progressive pain rather than an acute process. Others suggested features that increase the likelihood of Facet joint pain include age greater than 65, pain relieved by recumbency, absence of pain aggravation by coughing, forward flexion and aggravation by hyperextension.
Lumbar facet joint-mediated pain tends to present as a progressive pain rather than an acute process. Others suggested features that increase the likelihood of Facet joint pain include age greater than 65, pain relieved by recumbency, absence of pain aggravation by coughing, forward flexion and aggravation by hyperextension.
Upper lumbar facet joints tend to refer pain into the flank, hip and upper lateral thigh in comparison to the lower lumbar facet joints, where the pain may be experienced in the posterolateral thigh and occasionally as far distally as the calf.
The most useful physical examination finding is tenderness to palpation in the paraspinal regions.
SACROILIAC JOINT PAIN
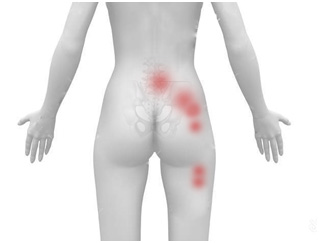 Patients with SI joint dysfunction will typically present with unilateral (4:1 vs. bilateral) pain. Pain is below the belt line and is exacerbated by activities such as rising from a seated position, getting out of a car, getting out of bed in the morning, and ascending stairs. They may describe hearing a popping, cracking, or clicking sound and experiencing groin or posterolateral thigh pain.
Patients with SI joint dysfunction will typically present with unilateral (4:1 vs. bilateral) pain. Pain is below the belt line and is exacerbated by activities such as rising from a seated position, getting out of a car, getting out of bed in the morning, and ascending stairs. They may describe hearing a popping, cracking, or clicking sound and experiencing groin or posterolateral thigh pain.
If the patient points to his sacral sulcus (positive Fortin finger sign) and demonstrates sacral tenderness on examination, the diagnosis of SI joint dysfunction is considered probable, and the clinician should perform special provocative tests, and consider diagnostic injections
LUMBAR SPINAL STENOSIS
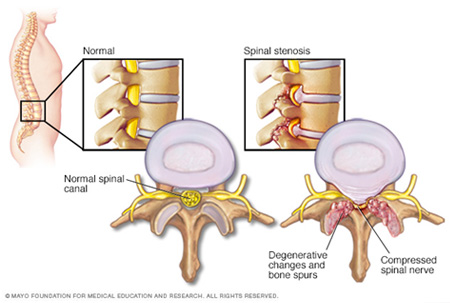 The pattern of pain in the lower back and legs commonly described as a 'heaviness' or 'deep aching' during standing or walking distinguishes neurogenic claudication associated with Lumbar spinal stenosis from other chronic Low back pain syndromes. This episodic pain problem is typically induced by erect postures and remits with lumbar flexion. The low back and leg symptoms associated with lumbar stenosis are characteristically "intermittent" to the extent that they are eased with sitting or lying down.
The pattern of pain in the lower back and legs commonly described as a 'heaviness' or 'deep aching' during standing or walking distinguishes neurogenic claudication associated with Lumbar spinal stenosis from other chronic Low back pain syndromes. This episodic pain problem is typically induced by erect postures and remits with lumbar flexion. The low back and leg symptoms associated with lumbar stenosis are characteristically "intermittent" to the extent that they are eased with sitting or lying down.
Physical examination findings most closely associated with this diagnosis are a gait with widened base, abnormal Romberg test , thigh pain following 30 seconds of lumbar extension, and neuromuscular deficits.
LUMBAR DISC DISPLACEMENT (sciatica)
 Patients experience radiating pain towards legs that may be described as sharp, dull, piercing, throbbing, or burning.
Patients experience radiating pain towards legs that may be described as sharp, dull, piercing, throbbing, or burning.
Forward flexion, sitting, bending or Valsalva maneuvers exacerbate symptoms . Lumbar extension may worsen pain if there is compromise of the spinal canal or foraminal space by the herniated disc. Additionally, dermatomal paresthesias are reported.
POSTLAMINECTOMY SYNDROME
Postlaminectomy syndrome, referred to as failed back surgery syndrome (FBSS). FBSS constitutes a heterogeneous group of disorders that occur post lumbosacral surgery and share pain as a common symptom.
PIRIFORMIS SYNDROME
TREATMENT OPTIONS
PHARMACOLOGICAL MANAGEMET PERCUTANEOUS DISCECTOMY FACET JOINT INJECTION ROOT SLEEVE INJECTIONS LUMBAR EPIDURAL INJECTION CAUDAL EPIDURAL INJECTION SI JOINT INJECTION
Surgical options:- These techniques are rarely required. There are specific indications for surgery. ONLY PAIN IS NOT AN INDICATION FOR SURGERY .

